Transurethral Resection of the Prostate
What is the prostate gland?
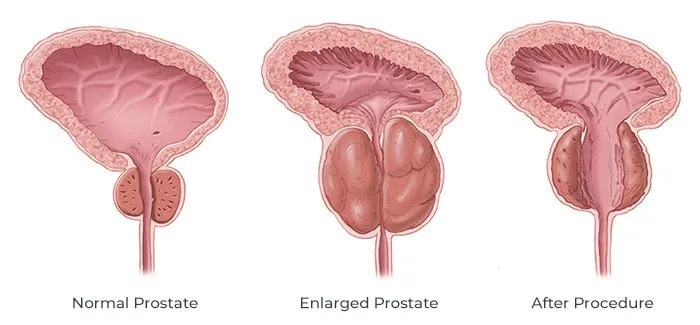
The prostate gland is a reproductive organ present in men. It sits at the outlet (base) of the bladder and surrounds the tube through which you pass urine (the urethra). It is like a doughnut with the ring being the urethra. Its role is to produce part of the semen (ejaculation) to provide nutrition to sperm from the testes.
Why is TURP necessary?
The prostate gland grows slowly throughout life. In some men it enlarges and can cause the following symptoms:
- Slower urine flow with dribbling.
- Reduction in strength of flow (not being able to hit the back of the pan).
- Needing to strain or push to pass urine.
- Feeling your bladder is not empty after you have finished urinating.
- Urinating more frequently with urgency (need to hurry to the toilet and sometimes with leakage).
- Getting up at night more frequently to pass urine.
- Difficulty starting and stopping the flow.
- Urine infection, blood in the urine, unable to pass urine at all with a catheter (plastic drainage tube) being placed in the bladder via the penis
If left untreated, the prostate can completely block the urethra and the outflow of urine. This is called acute retention and the bladder becomes stretched and painful. A tube must then be passed into the bladder via the penis to empty it. Even before complete blockage occurs, there may be complications like infection or damage to the kidneys.
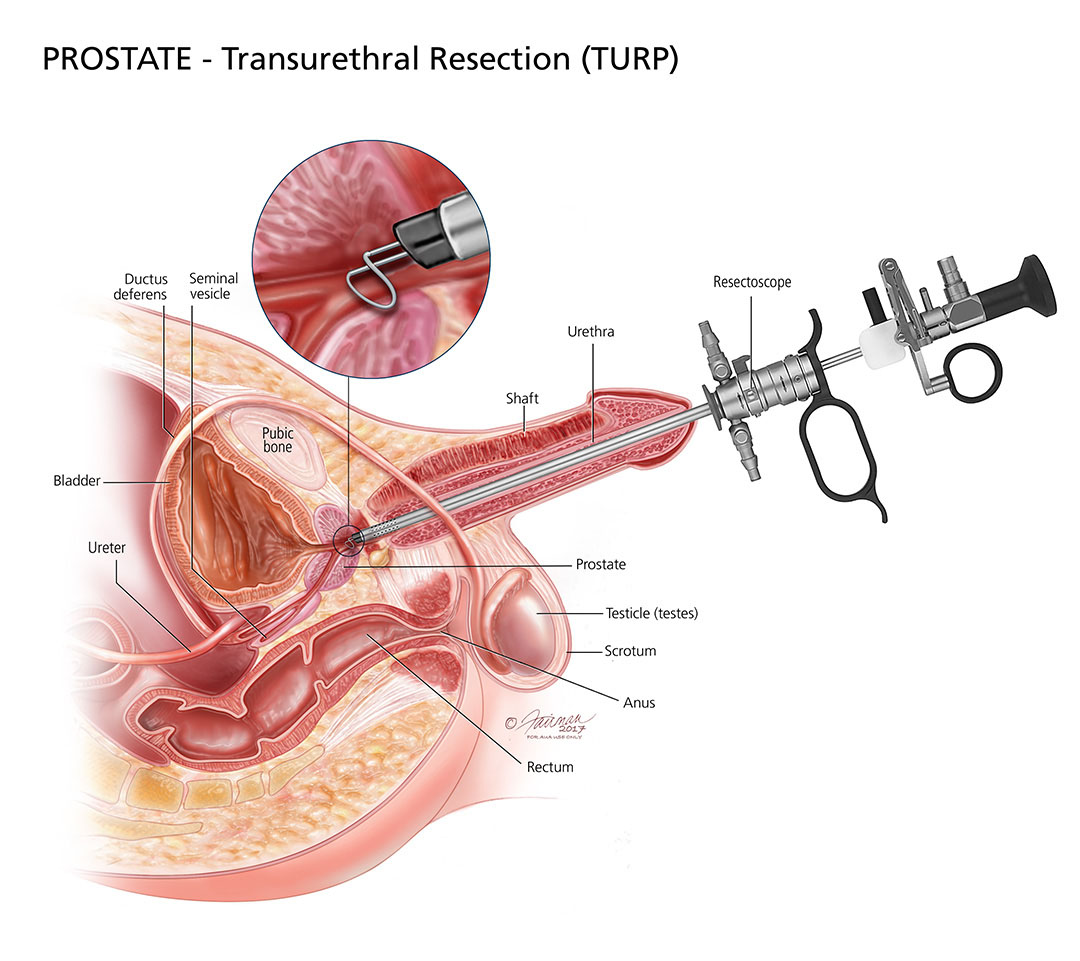
What does a TURP involve?
This is an operation to create a larger channel through the prostate gland. This will prevent or relieve obstruction to the flow or urine. During the operation, a small telescope is passed through the urethra (the tube through which you pass urine) and instruments are used to core out the inside of the prostate gland. There is no wound and no stitches are needed.
The operation will be done either with you asleep (general anaesthetic) or awake and numb from the waist down (spinal anaesthetic). The anaesthetist will discuss with you prior to the operation which option is best for you.
The length of the say in hospital varies from 2 to 4 days depending on your recovery and home circumstances.
What happens after the operation?
During the operation, the prostate tissue has been resected away, leaving a raw area that heals slowly over the next few weeks. While it is healing, the area will bleed. You will have a temporary plastic tube (catheter) coming out of your penis for approximately 48 hours. The catheter allows fluid to be passed up through the bladder to wash out blood and urine which drains into a bag. Do not be alarmed to see blood (coloured like red wine) in the catheter bag. This is normal.
Occasionally, a small blood clot can block the catheter and if you feel your bladder is full, please let the nursing staff know so they can flush the catheter to clear it. Catheter is removed after 2-3 days and you will be allowed to go home after a bladder scan (or suprapubic catheter) shows you can pass urine satisfactorily.
When you get home – what can I expect and what can I do?
>8 in 10 (80%) men will have a significant improvement in their overall urinary symptoms: better flow, less need to push to urinate, better emptying, less frequency, urgency & nocturia.
- Burning, stinging and blood in the urine and will improve with time.
- Frequency and urgency may temporarily worsen as the bladder still feels it needs to push hard to expel the urine and is unaware the obstruction (prostate) is now gone. This may be associated with urine leakage. Sometimes medications are required to decrease the bladders’ “overactivity”.
- Inability to pass urine occurs in a small proportion of men because the bladder has been stretched/strained for some time and it needs rest. In such a case, you may go home with a catheter to be removed as per Dr Menogue’s instructions. This occurs more often if there is already a catheter in before the operation for retention and success is less if complete blockage has occurred for a long time, i.e. chronic retention (=50%).
Bleeding:
You will see blood or small clots in your urine but this will settle over the next few weeks. It will be more noticeable on some days and especially in the mornings. A little extra bleeding is common 10-14 days after the operation as the scab formed in the prostate comes away.
Do not over exert yourself in the first month after the operation. This includes sex, strenuous exercise, e.g. running, swimming, cycling & golf. You may be prescribed medications to keep your bowels soft and regular.
Diet:
You can eat normally, but try to ensure a good intake of fruit and vegetables, and other high fibre foods, to help avoid constipation.
Continue to drink 2 litres of fluid each day for the first two weeks to continue the flushing process and to help prevent infection. Increase fluids if you notice the urine becoming more bloodstained. Alcohol is permitted in moderation.
Driving and Work:
Do not drive for 48 hours after the operation and only when you feel well enough. Usually it is safe to resume work 2-4 weeks after your surgery depending on the type of work you do. Please discuss with Dr Menogue
Possible Complications:
Any type of surgery has potential risks and complications. General complications relating to the anaesthetic or blood clots in the legs or lungs are very uncommon with this operation. Some of the more specific potential complications with TURP include:
- Retrograde ejaculation ‘dry orgasm’ (80%) Common but won’t affect your sensation or orgasm. The sperm flows back into the bladder rather than out of the penis. This is not harmful and the sperm will be passed the next time you urinate. This operation can therefore prevent you from fathering a child.
- Impotence (<5%) This is very uncommon but especially in older men or those with pre-existing problems with their erections, further reduction in the quality of the erections may occur.
- Heavy bleeding or blood clots requiring blood transfusion/ re-operation is uncommon but may occur (3%)
- Infections can be suggested by high temperature, ongoing burning or stinging or your urine becomes cloudy and smelly or your testicles become swollen or painful. These can all be treated with antibiotics which are also given during the operation to minimise your risk of this occurring.
- Permanent incontinence (<1%) due to injury or damage to muscles that control urine leakage is RARE. Early, temporary incontinence due to bladder overactivity (associated with urgency) can occur and will settle with time and may require medications initially (e.g. betmiga, vesicare, oxytrol).
- Fluid and electrolyte abnormalities (<1%) relate to absorption of irrigating fluid and is RARE.
- Finally, about 1 in 5 men within 10 years of their operation (TURP) will need a further operation as the prostate tissue re-grows or narrowing in the urethra occurs. The prostate is never completely removed in this operation and so it is important to still be tested for prostate cancer.
Follow Up:
Arrange to see Dr Menogue approximately 6 weeks after your operation for review and the results of the prostate samples to test for cancer will also be discussed.